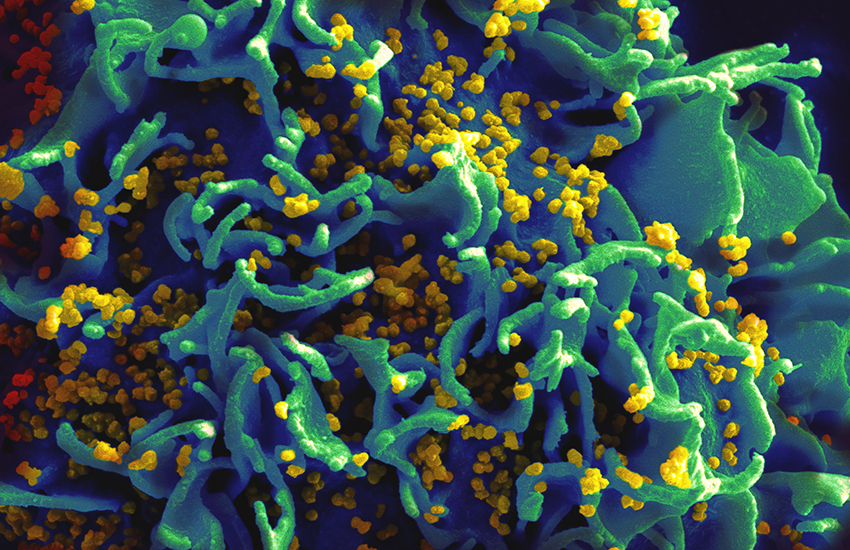
This is what HIV looks like when it infects a cell
Immediate action must be taken to slow new HIV infections among Australia’s Aboriginal and Torres Strait Islander people.
Researchers have argued that the government introduce ‘an accelerated HIV prevention and control strategy’.
New data has revealed a 33% increase in new HIV diagnosis rates among Indigenous people between 2012 and 2016.
But what is shocking is that in the same period, newly diagnosed HIV rates among Australian-born non-Indigenous people decreased 22% .
A new article in the Medical Journal of Australia released this week revealed the worrying trend. The article said for the first time since 1992 – when HIV data started being recorded – rates of new HIV cases in Aboriginal people were double that of non-Aboriginal people.
The articles authors; James S. Ward, Karen Hawke and Rebecca J. Guy argued that it was crucial to act immediately.
‘Acting now to avoid HIV becoming a concentrated epidemic among Aboriginal and Torres Strait Islander people should be a national priority,’ they wrote.
‘HIV in Australia is currently considered to be a low-level epidemic, but there is general consensus that it could rapidly transition to a concentrated epidemic among Aboriginal and Torres Strait Islander people, as has occurred among First Nations people in some provinces of Canada.’
Slow uptake of PrEP
If something was not done soon to stop new HIV cases, it could effect Australia’s target of no new HIV transmissions by 2020.
But they did explain some of the reasons why the rates of new HIV cases were so high. Some of the reason included; poorer outcomes for many of the socio-cultural determinants of health, particularly education, income, unemployment, racism and access to health services.
Aboriginal people were also less likely to be involved with biomedical HIV prevention interventions. Those interventions include; treatment as prevention (TasP) and pre-exposure prophylaxis (PrEP).
‘Of the almost 17 000 people enrolled in PrEP trials in Australia, about 200 are Aboriginal and Torres Strait Islander people, thus leaving a gaping hole in evaluation of this new prevention strategy for this population,’ the article reads.
Different HIV populations
Another reason why the HIV rates were so high among was because it affects different populations to non-Aboriginal people.
Compared with non-Indigenous people, a lower proportion of HIV diagnoses have occurred among men who have sex with men.
But a higher proportion of diagnoses occur in people who inject drugs, 14% in Aboriginal populations compared to 3% in non-Aboriginal populations.
Heterosexual Indigenous people were also more likely to acquire HIV. The rate of new cases in Aboriginal women is also three times higher than non-Indigenous women.
What to do
The researchers called for immediate action. They recommended that there needs to be ‘greater recognition that the intersectionality of the social and cultural determinants of health drives differentials in HIV’.
The article also recommends increasing HIV testing. But it also called to increase PrEP access for people at greatest risk of acquiring HIV in Indigenous populations.
‘Acting now to avoid HIV becoming a concentrated epidemic among Aboriginal and Torres Strait Islander people should be a national priority,’ the article reads.
‘Immediate changes are necessary to ensure that the elimination of HIV in Australia includes Aboriginal and Torres Strait Islander people.’